Discussion: Scans And X-rays – Useful or Not Useful?
Do you think I need an X-ray?"
This is an extremely common question we get asked by our patients, almost daily. And, rightly so – we love it when you ask questions. It tells us that:
a) You feel like you’re in a safe enough environment to ask and discuss it, and
b) You’re interested in your body.
Well, we are interested in your body too. And sometimes, the answer is ‘yes’ – we should (and do) send you for an X-ray.
We’ll do this if we think it is going to either add something to our diagnosis or treatment plan, or if we want to rule something out (or to be “less likely” in the world of medicine – nothing is ever “ruled out”).
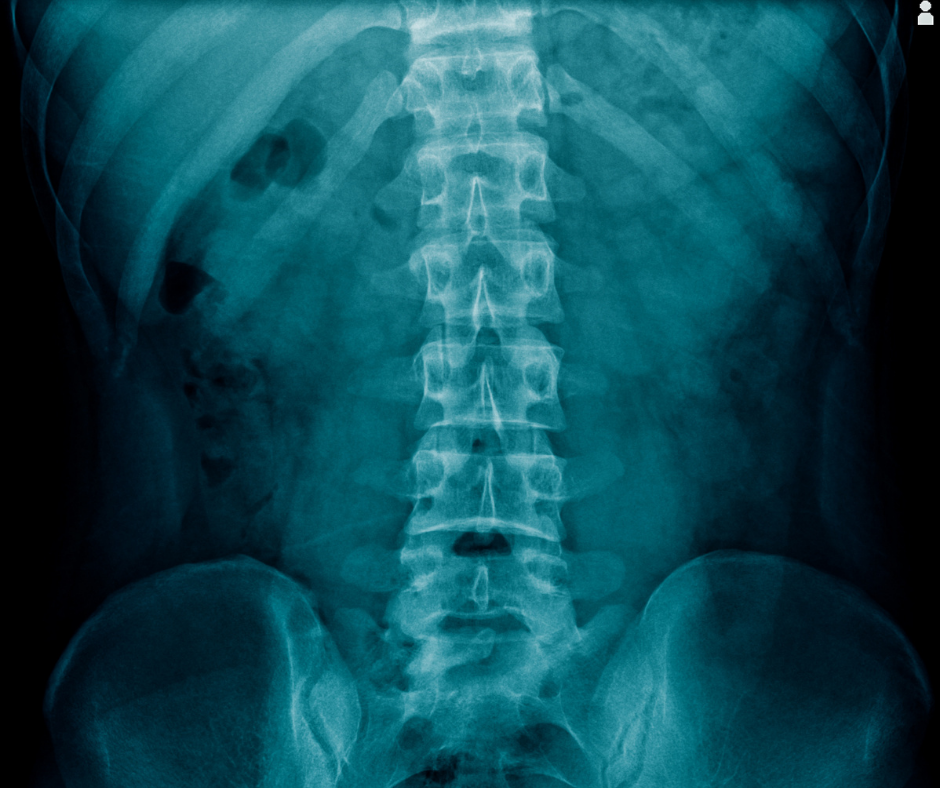
There are many times we are asked to send patients for an X-ray if they think or have been told they’ve got arthritis. If we think you’ve got arthritis, we won’t always send you for an X-ray.
And here’s why: The report will say “mild / moderate / severe arthritis”. We knew that (or suspected it). We haven’t necessarily gained anything helpful to relieve your pain.
Now, this might be relevant if we’re thinking of sending you to a specialist for further assessment, or, in the case of the spine, if we think that arthritis has led to you having some kind of instability. We do like to check for this when we’re treating you, as it could influence the types of techniques we select to get you better.
Just because an X-ray shows you've got Arthritis, it doesn't mean that the Arthritis is necessarily the cause of your pain

If an X-ray has shown marked arthritis, then yes, it is likely to be adding to your pain. But the term arthritis mean inflammation of the joint (“Arthrosis”) – you also have ligaments, tendons, and muscles that may be involved, all of which could also be (or independently be) the source of your pain.
So take this with a grain of salt.
Here's some examples of when an X-ray is REALLY useful.....
- When we want to send to you a specialist. They need to most up to date pictures of your back / knee / shoulder or body part before they’ll see you most of the time.
- When we think something may actually have been broken, or if you might have an unhealed fracture.
- If we’re worried about the shape of your spine – either side to side, or front to back (or occasionally both).
- If we think there is a type of instability in your back or neck called a Spondylolisthesis / Retrolisthesis / Anterolisthesis – where one of the vertebrae has slipped slightly forwards or backwards. This will have a big impact on our treatment of you, and also for your future safety with us or any other practitioners who manage your issues.
So what about Ultrasound Scans?
Ultrasound scans can be really useful to us as Osteopaths, especially around the shoulder. In fact, we’ll often send people with shoudler problems, that dont respond as well as we’d like for a scan within treatments 1 to 2. We like to ascertain whether the shoulder muscles are in tact , or not, or if they are partially intact. BUT … here’s where it gets really interesting. From an Osteopathic point of view, we’re looking at what we can do to improve you, exactly as you are (i.e. intact or not. Or, with arthritis, or not).
The presence of a tear on ultrasound especially at the shoulder, gives us more of an indication as to how quickly we (you and us) can expect you to get better, and what exercises to give you to increase your response to treatment / return to function.

A significant proportion of the population have shoulder muscle tears which are asymptomatic - the patient has no pain or problem from this tear.
Therefore, again just because a tear (or partial tear) shows up on an ultrasound scan, it doesn’t necessarily mean it is causing the problem you came to us with initially. If something is not intact anymore (i.e. torn or partly torn) then it will not perform 100% correctly and other muscles and ligaments etc. will be recruited to perform the same function of the arm. Plus, you’ll likely have reduced strength for certain activities.
BUT… this doesn’t really matter for everyone, as long as you can do the things you need to do in life. Not all of us need to do handstands or backflips for a living, and we’re quite content to do a bit of tennis, gardening etc.
Again, what matters to us as osteopaths is :
a) What can we do to alleviate your pain?
b) What do you, the patient, need to be able to do in life for both essential skills (like washing under your arm pit) and desirable skills (like an overhead serve in tennis or putting your arm up in dancing class)?
When we’ve determined this, we can ascertain if we can get you there, or at least partly there, and what you can do to help yourself maintain good function for a pain-free or pain less life.
We do this for you whether there is a tear or not.
"Wouldn't 'they' want to do surgery for a shoulder muscle tear?"
Sometimes ‘yes’, and sometimes ‘no’. This is largely relevant to how much pain a patient is in and the lifestyle choices the patient wishes to make. Age has some influence, but it isn’t everything. There are young people who want to do hang gliding and rock climbing, and there are mature people who want to do just the same. If the tear is a complete thickness tear in a younger person, then surgery may be considered. Surgery may also be necessary if the muscle tear has reached the articulating (deep) surface of the joint.
This is not something we can advise you on, and in this instance we would refer you to a specialist for further investigation. They are the ones with the most up to date knowledge and can advise you of the best possible outcomes for you shoulder, which may or may not be a surgical option.
Here's how we manage your pain or problem at ThreeSixty...
We listen to your story:
- What happened?
- What can’t you do?
- What do you want to get back to doing?
We observe and assess:
- What you can do
- What you can’t do
- What you ‘should’ be able to do (for your age and general fitness level)
We make a plan together, on how to get you back to doing what you love.

Disclaimer: All information presented on this page is intended for informational purposes only and not for rendering medical advice. The information contained herein is not intended to provide medical advice, diagnose, treat, cure, or prevent any disease. It is the opinion of the author alone.
Share This Post
Subscribe to Our Newsletter
Get updates and learn from the best
More to Explore




Want To Keep Moving?
SDrop Us A Line And Keep In Touch



